Definition of Herpes Zoster
Herpes zoster, also called shingles, infects the skin and nerves, producing red patches, blisters, and vesicles that cluster along peripheral nerves. The reactivation of the latent Varicella zoster virus (VZV) in the sensory nerve roots near the spinal cord causes this disease.
Older adults and individuals with weakened immune systems, especially those with HIV/AIDS, commonly experience this condition.
Etiology
The Varicella zoster virus (VZV) causes two distinct conditions: chickenpox and herpes zoster. When the virus reactivates, it travels backward from the sensory ganglia along the nerve cells and spreads through the epidermis, causing neurological and mucocutaneous symptoms.
Symptoms of Herpes Zoster
Prodromal Stage: The disease initially presents with abnormal sensations on a localized skin area, such as burning, tingling, numbness, or pain, particularly at night. Rarely, there might be paresthesia in one or multiple nerve distributions, lasting from 1 to 5 days. Moreover, accompanying symptoms may include headaches, photophobia, and discomfort. This stage likely represents the virus spreading along the nerve pathways.
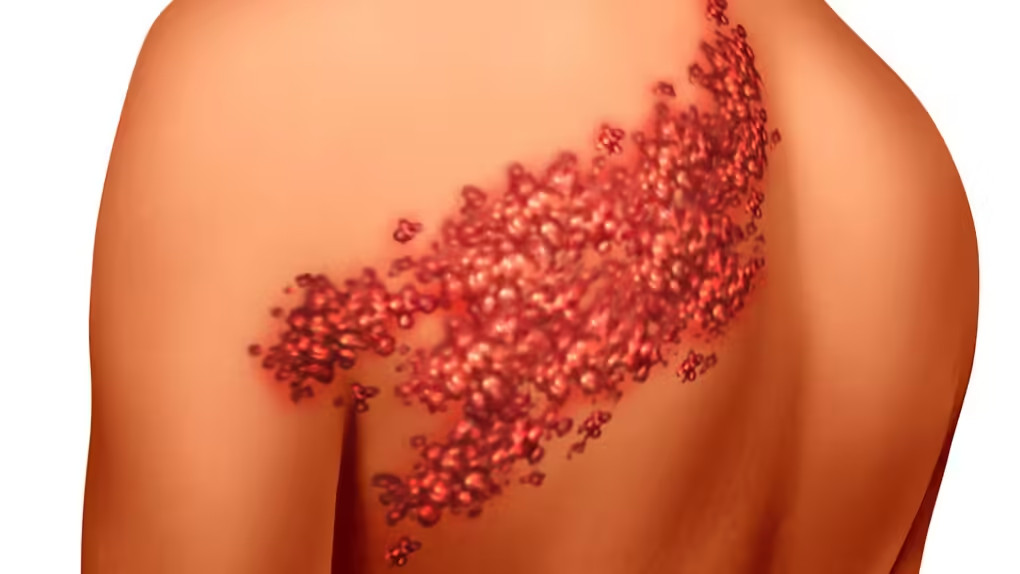
Onset: About half a day later, red patches with slight swelling, a few centimeters in diameter, appeared on the skin area and showed prodromal signs. Normally, These patches are slightly raised and follow the nerve distribution, gradually merging to form stripes or bands.
Full-Blown Stage:
- Skin Symptoms: A few days later, vesicles and blisters appear on the red patches, clustered like grapes. Initially, the vesicles are tense and filled with clear fluid, which later becomes cloudy and purulent. These blisters eventually rupture, forming crusts. The average duration from the appearance of lesions to scar healing is around 2 to 4 weeks.
- In the Elderly: The lesions are more extensive, covering a larger area, and the vesicles and blisters may become hemorrhagic, leading to skin necrosis, infection, and unsightly, prolonged scarring.
- In Children, The lesions are typically less extensive and heal more quickly.
- Location: The lesions usually appear on one side of the body, do not cross the midline, and follow the distribution of a peripheral nerve. However, In rare cases, they may affect both sides or become widespread.
- Lymph Nodes: Nearby lymph nodes may become enlarged.
- Functional Symptoms: Pain typically occurs early and can precede the skin lesions, varying throughout the disease course. The intensity of the pain ranges from mild, like a burning sensation or local discomfort, to severe, like stabbing or shooting pains.
- Pain Variation with Age: Pain is usually mild in children and young adults. However, in older adults, pain can be severe and prolonged, sometimes persisting for years after the skin lesions have healed, a condition known as postherpetic neuralgia.
- Other Disorders: There may be disturbances in sweating, vasomotor function, or piloerection (hair standing on end), although these are rare.
Diagnosis Herpes Zoster
Definitive Diagnosis of herpes zoster: Shingles (herpes zoster) is primarily based on clinical symptoms.
Clinical Forms:
- Based on the Location of Lesions:
- Intercostal and Abdominal Shingles: This is the most common clinical form, accounting for 50% of cases.
- Cervical Shingles (Superficial Cervical Plexus) and Cervico-Brachial Shingles.
- Nape of the Neck Shingles: Involves the nape, scalp, and auricle.
- Shingles of the Hip, Abdomen, Genitals, Groin, Sacrum, Ischium, and Thigh.
- Based on the Morphology of Lesions: These forms are typically seen in immunocompromised individuals, such as those with HIV/AIDS, cancer, or undergoing chemotherapy, and include:
- Disseminated Zoster.
- Multiple Nerve Zoster.
- Recurrent Zoster.

Unique Forms of Shingles:
- Ophthalmic Zoster: Accounts for 10-15% of shingles cases. The V or trigeminal nerve, which innervates the eye, upper jaw, and lower jaw, becomes involved, with the ophthalmic branch being affected five times more frequently than the others. Potential eye complications include conjunctivitis, keratitis, scleritis, and, in severe cases, sight-threatening conditions like acute retinal necrosis, optic neuritis, orbital apex syndrome, posterior scleritis, and secondary glaucoma.
- Geniculate Ganglion Zoster or Ramsay Hunt Syndrome: Caused by damage to the geniculate ganglion of the VII cranial nerve. Patients experience unilateral facial paralysis, tinnitus, hearing loss or deafness, nausea, vomiting, vertigo, and nystagmus. The eye on the affected side cannot close completely (Bell’s phenomenon), and there may be a loss of taste sensation on the anterior two-thirds of the tongue. Vesicles appear on the tympanic membrane, ear canal, and auricle. Moreover, encephalitis and meningitis may occur.
- Sacral Shingles (S2, S3, S4): Involves inflammation of the nerves that control the bladder, leading to difficulty urinating, urinary frequency, urinary retention, and, in some cases, hematuria or pyuria. Patients may experience abdominal pain similar to surgical conditions, with lower abdominal cramps, fullness, constipation, and a spastic and rock-hard anal sphincter, making rectal examination impossible. Pain and typical skin lesions are also on one side of the genital area.
- Ear Shingles: Causes burning pain in the ear, which can spread to the temple and nape of the neck. The pain occurs in bouts lasting several days, making it difficult for the patient to eat or sleep, especially when combined with throat shingles, leading to painful swallowing. There may also be facial sensory disturbances, peripheral facial paralysis, and hearing loss.
- Shingles in HIV/AIDS Patients: In the early stages of HIV infection, shingles manifest similarly to shingles in non-HIV-infected individuals. However, in the late stages of HIV/AIDS, shingles may recur frequently and present atypically, with widespread lesions, hemorrhagic vesicles, necrosis, infection, unsightly scarring, and prolonged disease duration.
Paraclinical:
- Tzanck Cell Test: Identifies acantholytic cells and multinucleated giant cells.
- Viral Culture: Rarely performed.
- PCR: Conducted on samples from vesicular fluid and tissues.
- Skin Biopsy: Performed if clinical presentation is atypical.
- HIV Testing.
Differential Diagnosis: Depending on the stage of the disease
- Prodromal Stage: Differentiates from other types of pain such as headaches, iritis, pleuritis, brachial neuritis, cardiac pain, appendicitis, cholecystitis, gallstones, renal colic, herniated discs, and sciatica.
- Vesicular Stage: Differentiates from herpes simplex, allergic contact dermatitis (from certain plants and insects), and, more rarely, autoimmune blistering diseases such as pemphigus, pemphigoid, Duhring-Brocq disease, and linear IgA disease.
Treatment
Therapy Goals: Promote healing of lesions, reduce pain, and prevent complications.
Treatment Protocol
- For uncomplicated cases and individuals with normal immunity: Topical treatment: Apply water-based ointments, Millian’s solution, Castellani’s paint, acyclovir ointment, and antibiotic ointment if there is a secondary infection.
- Medication treatment:
- Antiviral drugs (Acyclovir, Famciclovir, Valacyclovir): These antivirals accelerate wound healing, reduce the number of new lesions, and alleviate postherpetic neuralgia. The medication should be administered early, preferably within the first 72 hours.
- Antibiotics in case of secondary infection (Augmentin, Cefuroxime).
- Pain relief: Commonly used medications include neuropathic pain relievers (Carbamazepine, Gabapentin, Pregabalin) and B vitamins.
- Topical application of creams containing corticosteroids and anesthetics such as lidocaine or prilocaine.
- Corticosteroids (Methylprednisolone, Betamethasone) help reduce pain during the acute phase, and many experts believe these drugs also reduce postherpetic pain.
It is recommended to combine different treatment methods to achieve the best outcomes for patients suffering from postherpetic neuralgia.
Combining acupuncture and other traditional medicine treatments has proven highly effective in managing pain.
Prevention
Avoiding VZV (Varicella-Zoster Virus) infection is the best way to prevent shingles. However, for adults who had chickenpox during childhood and have latent VZV, the preventive strategy against VZV reactivation is vaccination.
Additionally, boosting the immune system is an indirect method to prevent VZV reactivation. Maintaining a balanced diet, leading a healthy lifestyle, and regular physical exercise can strengthen the immune system.