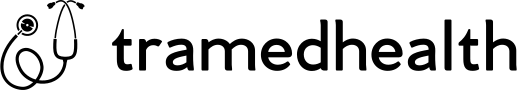
Definition of Osteoporosis
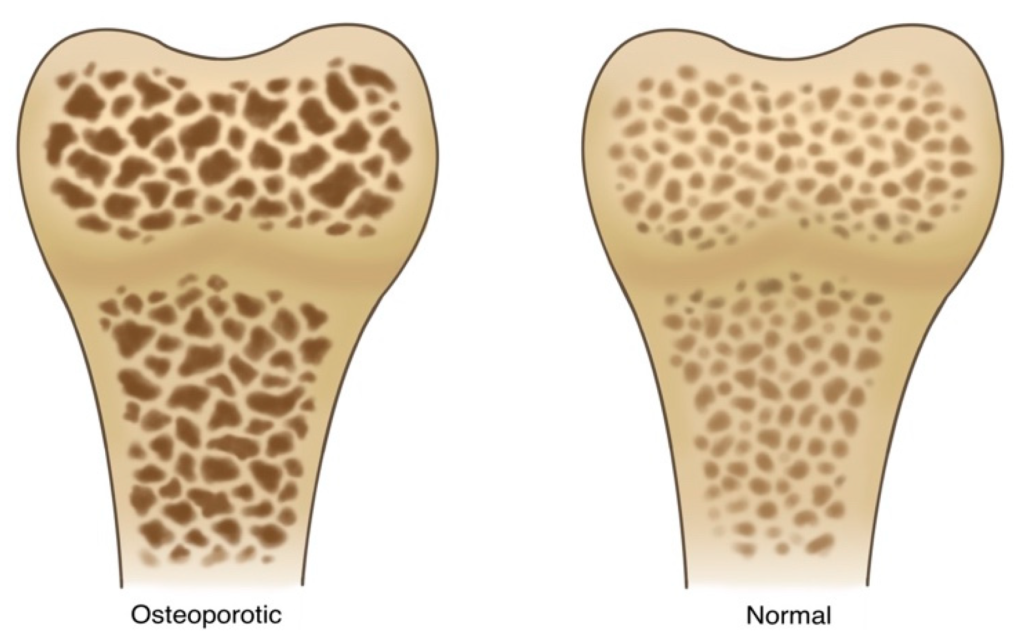
Osteoporosis is a metabolic bone disorder, which consequently results in impaired bone strength and an increased risk of fractures. Specifically, bone strength encompasses the integrity of bone mass, including bone mineral density and bone mass. Additionally, it involves bone quality, which encompasses bone volume, bone microarchitecture, and bone turnover.
Causes of Osteoporosis
- Osteoporosis in older adults (Primary osteoporosis)
Primary bone loss often appears late, progresses slowly, increases gradually, and has few severe complications such as fractures or vertebral collapse.
- Postmenopausal osteoporosis
Postmenopausal reduced bone density worsens age-related osteoporosis in women due to a sudden decrease in estrogen during menopause.
- Secondary osteoporosis tends to become more severe earlier and is associated with more complications if the patient has one or more of the following risk factors:
- Firstly, poor physical development since childhood can contribute to the progression of bone loss. Additionally, a family history of parents with weak bones or fractures can increase the likelihood of developing the condition.
- Moreover, insufficient physical activity, limited outdoor activities, and long-term immobility due to illness or occupation are significant risk factors. Furthermore, habitual use of alcohol, beer, coffee, and tobacco negatively impacts bone health.
- In addition, long-term use of certain medications, such as corticosteroid anti-inflammatory drugs and diabetes medications, can exacerbate the condition. Finally, suffering from certain diseases, including endocrine disorders and gonadal insufficiency in both males and females, can also significantly increase the risk of bone loss.
Symptom
Weak bone is a silent disease with no specific clinical symptoms, only manifesting when complications occur.
- Acute and chronic bone pain and back pain. A feeling of heat and cold deep in the bone may accompany it.
- Spinal deformity: Hunchback, scoliosis, reduced height due to fractures of the vertebral bodies.
- Chest pain, difficulty breathing, slow digestion due to effects on the chest and vertebral bodies.
- Fractures: Common locations are fractures of the distal end of the radius, fractures of the femoral neck, and fractures of the vertebrae (back and lumbar), occurring after mild trauma, even without apparent trauma.

Diagnosis
Because there are no specific clinical symptoms, osteoporosis is usually diagnosed only when symptoms are as above or accidentally detected during a general examination or other musculoskeletal diseases. Necessary paraclinical tests include:
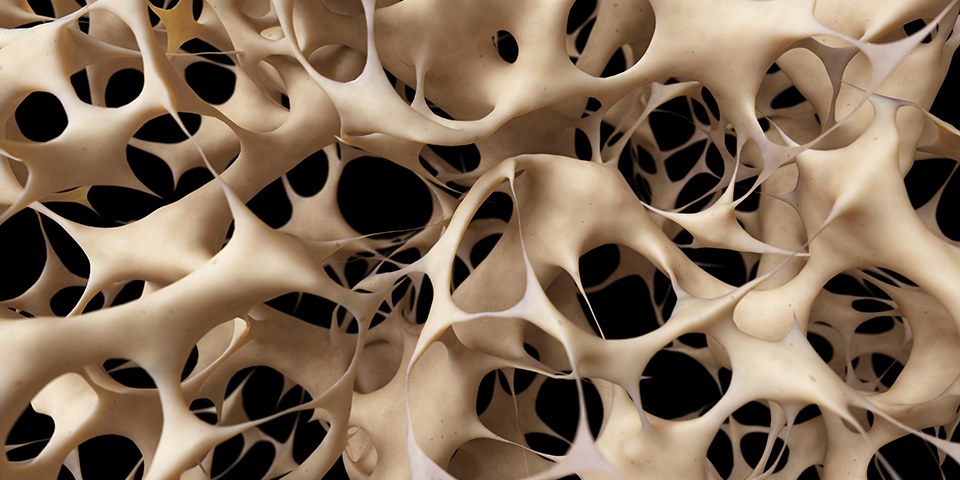
- Conventional X-ray: images of the vertebrae with increased radiolucency, vertebral body deformation (fractures cause collapse and subsidence of the vertebrae), with long bones often reducing the thickness of the bone cortex (causing the medullary canal to widen).
- Measuring bone mass (BMD) by Dual Energy X-ray Absorptiometry (DXA) at central locations such as the hip joint or lumbar spine to diagnose osteoporosis, assess the degree of osteoporosis, predict the risk of fracture, and monitor treatment.
- Some other methods: CT Scan or MRI can be used to assess bone mass, especially in the spine or femoral neck.
The World Health Organization (WHO) 1994 criteria for diagnosing osteoporosis, measuring bone density at the lumbar spine and femoral neck using the DXA method:
- Normal bone: T score from -1SD or higher.
- Osteopenia: T score below -1SD to -2.5SD.
- Osteoporosis: T score below -2.5SD.
- Severe osteoporosis: T score below -2.5SD with a history/current fracture.
Differential diagnosis
- Osteogenesis Imperfecta (OI).
- Secondary osteoporosis, such as bone metastases and malignant diseases of the hematopoietic system (multiple myeloma, leukemia, etc.).
Treatment for Osteoporosis
- Non-drug treatment
- Diet: Supplement calcium-rich foods (according to the body’s needs: from 1,000-1,500mg daily, from sources: food, milk, and pharmaceuticals)
- Avoid risk factors: tobacco, coffee, alcohol. Avoid being overweight or underweight.
- Lifestyle: Increase exercise, increase muscle flexibility, and avoid falls.
- Use tools and orthopedic braces (for the spine, for the hip joint) to reduce pressure on the spine, bone heads, and hip bones.
- Drug treatment
- Supplements if the diet is inadequate (daily use during treatment).
- Calcium: need to supplement calcium 500 – 1,500mg daily
- Vitamin D 800 – 1,000 IU daily.
- Anti-osteoclasts: Reduce osteoclast activity: Alendronate, Zoledronic acid, Calcitonin.
- Dual-action drugs: Strontium ranelate
- Symptomatic treatment
- Prescribe stepwise analgesics when necessary.
- Neuropathic pain relievers, B vitamins.
- Surgical treatment of complications of femoral neck fractures and vertebral body fractures.
Prevention
Osteoporosis is a preventable disease:
- Provide adequate calcium, vitamin D, and other essential nutrients for the body throughout life, according to the needs of each age and physical condition.
- Maintain a regular exercise regimen to help store calcium for bones and increase dexterity, muscle strength, and balance to reduce the risk of falls and fractures.
- Limit some habits: smoking, drinking too much alcohol, coffee, and exercising little.
- When the patient is at risk of osteoporosis (BMD from -1.5 to – 2.4 SD) but has many risk factors: must use corticosteroids to treat underlying diseases, family history of osteoporosis fractures, high risk of falls…, bisphosphonates can be prescribed to prevent osteoporosis.