Definition of Rheumatoid Arthritis
Rheumatoid arthritis is a typical autoimmune disease with chronic progression, with joint, extra-articular, and systemic manifestations at various levels.
The disease has a complex progression, causing severe consequences, so it needs to be actively treated from the beginning with effective treatment measures to stop or slow down the progression of the disease, limit disability, and improve the quality of life for patients.
Causes of Rheumatoid Arthritis
- The disease has an unknown cause related to infection, genetics (female, middle-aged, HLA factors), and immune response disorders.
- In which the role of B lymphocytes (humoral immunity), T lymphocytes (cell-mediated immunity), and macrophages with the participation of autoantibodies (anti-CCP, RF) and cytokines (TNFα, IL6, IL1).
Symptom
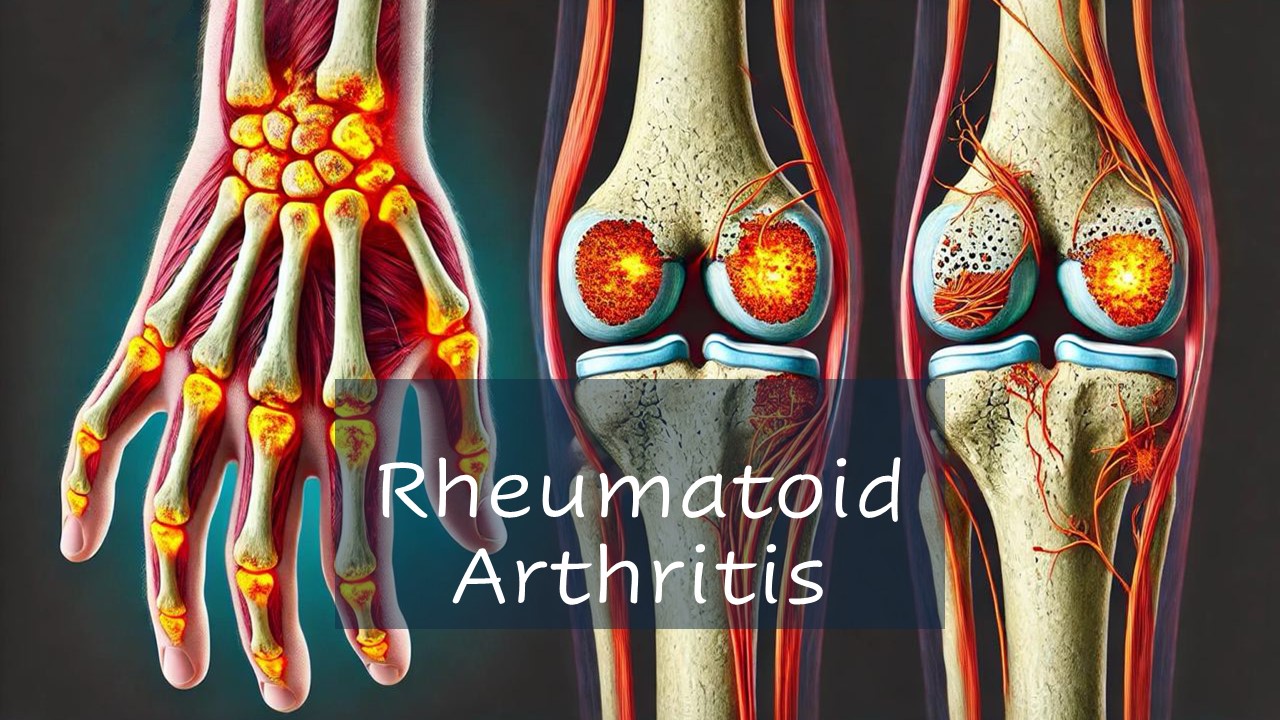
Early signs of rheumatoid arthritis
- Morning stiffness.
- Mild inflammation of a few joints in the limbs. In middle age, muscle pain is often easily confused.
- Duration from a few days to a few weeks.
- The time to confirm the diagnosis of RA is usually at least six months after the onset of the disease; in many cases, the diagnosis is late, possibly many years.
General signs
- Whole body: Weight loss, fever, fatigue, loss of appetite, insomnia, numbness in the extremities, sweating a lot
Joint manifestations
- Morning stiffness ≥ 1 hour
- Synovitis of peripheral joints, common locations such as finger joints, metacarpophalangeal joints, wrist joints, elbow joints, toe joints, metatarsophalangeal joints, ankle joints, and knee joints.
- Usually symmetrical
- May involve knee or wrist effusion
Reversible signs and symptoms associated with synovitis
- Morning stiffness
- Inflammation (swelling, heat, redness, and pain) of peripheral joints
- Joint effusion (usually bilateral)
Irreversible signs and symptoms
- Functional and anatomical deterioration of the joint
- Damage to articular cartilage, bone ends, tendons, and ligaments
Diagnosis
American College of Rheumatology (ACR) 1987 criteria
American College of Rheumatology/European League Against Rheumatism 2010 criteria (ACR/EULAR 2010 – American College of Rheumatology/European League Against Rheumatism)
Necessary paraclinical tests:
- Rheumatoid factor RF (Rheumatoid Factor): positive in 50-75% of patients with RA.
- Anti-cyclic citrulline peptide (Anti CCP): positive in 70-80% of patients with clearly diagnosed RA and 50% in early RA.
- Blood count: decreased red blood cell count, increased platelets, and a mild increase in white blood cells are the most common signs.
- Erythrocyte sedimentation rate (ESR): assesses inflammation or disease activity and monitors disease progression and response to treatment.
- CRP: often increased in inflammatory, autoimmune, and infectious diseases. If CRP is very high in patients with RA, the possibility of secondary infection should be carefully considered.
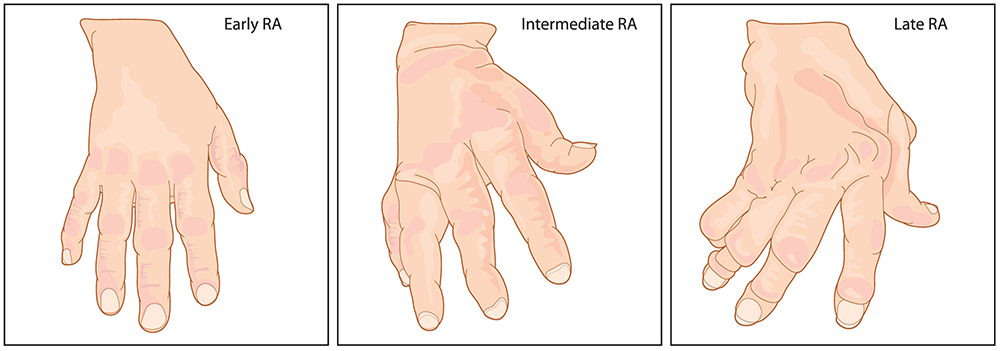
- X-ray: erosive lesions at the bone ends that gradually worsen with the progression of the disease; more severe are images of articular cartilage erosion, narrowing of the joint space, misalignment, dislocation, and secondary degeneration.
- Joint ultrasound, doppler ultrasound: assess the state of synovitis.
- Bone mineral density measurement (BMD): assess bone mass, diagnose osteopenia-osteoporosis, and fracture risk in patients with RA.
Differential diagnosis
- Systemic lupus erythematosus
- Osteoarthritis
- Chronic gouty arthritis and pseudogout
- Ankylosing spondylitis
- Psoriatic arthritis
- Infectious arthritis (including joint tuberculosis)
Treatment
Treatment principles: Active, comprehensive, and long-term treatment from the beginning, including:
- Symptomatic treatment with anti-inflammatory drugs, reducing the dose to maintain the lowest effective dose.
- Basic treatment with classic DMARDs, biological drugs depending on each patient.
- Restoring joint function.
- Monitoring, preventing, and treating the disease and treatment complications.
Non-drug treatment
- Maintain a reasonable diet rich in vitamins and minerals and full of amino acids necessary for the body. Limit sugar, starch, saturated fat, and salt, and do not smoke.
- Patients must have a regular exercise and movement regimen to prevent muscle and tendon contraction, joint adhesion, and muscle atrophy.
- During acute inflammation, let the joint rest in a functional position, avoid improper padding at the joint, and use orthopedic braces to avoid joint contraction at night.
- Encourage patients to exercise when inflammation symptoms subside, gradually increase, many times a day, suitable for each patient.
- Health education encourages patients to comply with treatment regimens, exercise, and monitoring.
Drug treatment
Symptomatic treatment: to improve inflammation symptoms, reduce pain, and maintain mobility (but not change the disease progression). Commonly used drug groups include:
- Non-steroidal anti-inflammatory drugs (NSAIDs): Diclofenac, Meloxicam, Celecoxib.
- Corticosteroids (prednisolone, prednisone, methylprednisolone)
- Simple pain relievers: Paracetamol/tramadol/codeine.
- Basic treatment with disease-modifying anti-rheumatic drugs (Disease Modifying Anti-Rheumatic Drugs) to slow or stop the progression of the disease, requiring long-term treatment and monitoring of clinical and paraclinical symptoms throughout the treatment period):
- Classic drugs: methotrexate (MTX), sulfasalazine (SSZ), hydroxycloroquine (HCQ), Leflunomide.
- Biological drugs: anti-interleukin 6, anti-TNFα, anti-B lymphocytes, anti-T lymphocytes, anti-interleukin 1.

Prevention
- There is no specific preventive measure; active preventive interventions for rheumatoid arthritis are general measures to improve health and physical condition, including diet, exercise, work, and avoiding stress.
- Avoid living and working in humid environments for a long time.
- Early detection of infectious diseases and immune disorders.