Introduction
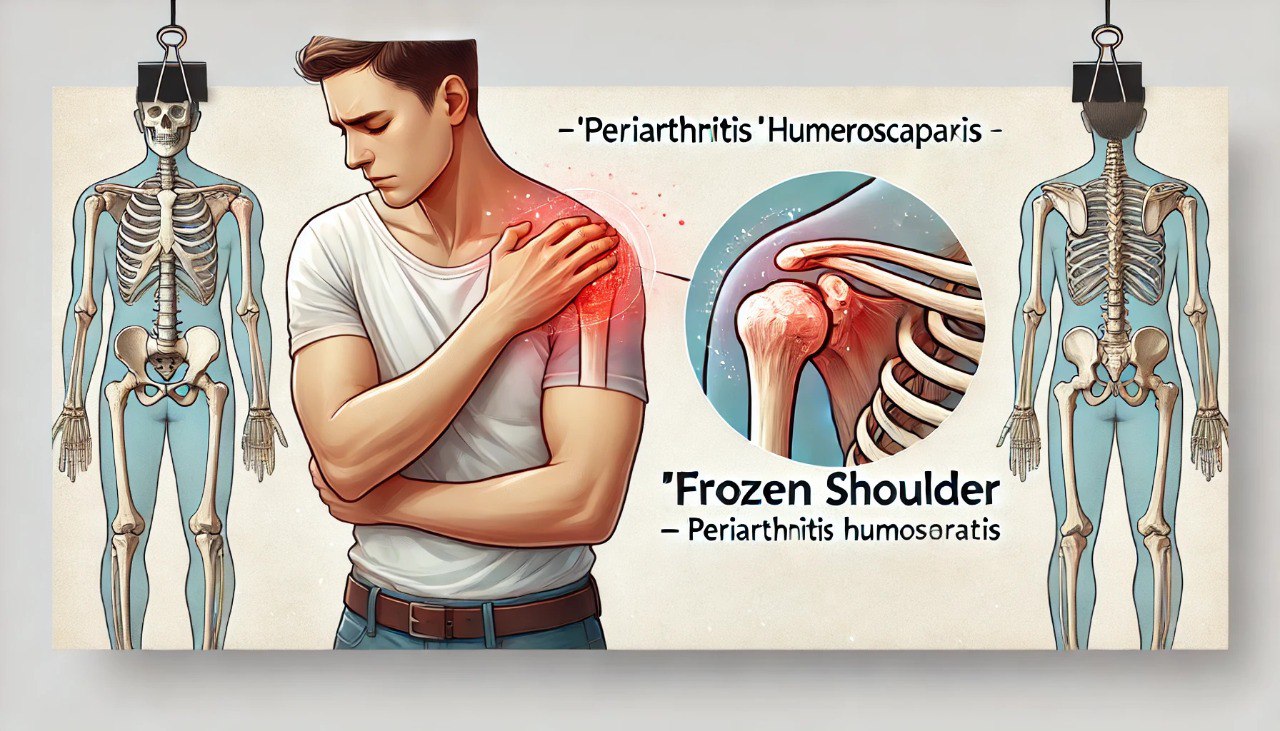
Periarthritis of the shoulder is a shoulder joint disease commonly found in the elderly or people who use the shoulder joint a lot. It typically has symptoms such as pain, stiffness, and limited shoulder joint movement.

Definition
Periarthritis humeroscapularis is a general term used for inflammatory diseases of the soft tissue structures around the shoulder joint: tendons, bursae, and joint capsule, not including diseases that damage the bone head, articular cartilage and synovial membrane such as infectious arthritis, rheumatoid arthritis, etc.
Causes
- Age-related tendon degeneration: The disease often occurs in people over 50.
- Heavy labor occupations with repetitive mechanical injuries cause damage to the tendons around the shoulder joint, such as the supraspinatus tendon and biceps brachii.
- Excessive exercise, such as playing sports that require lifting the arms above the shoulder, such as badminton, tennis, basketball, and volleyball.
- Shoulder injuries are due to falls, slips, and car and motorbike accidents.
- Some other diseases (cardiovascular, respiratory, diabetes, breast cancer, neurological, sleeping pill abuse).

Symptom
Depending on the cause and location of the injury, there are often the following symptoms:
- Simple shoulder pain (chronic tendonitis):
Shoulder pain often appears after excessive shoulder movement or after consecutive microtrauma in the shoulder joint—mechanical pain. Pain increases when performing antagonistic arm flexion movements. There is little limitation of joint movement. Often occurs with damage to the biceps tendon and supraspinatus tendon. There is usually a sharp pain point when pressing at the attachment point of the long bundle of the biceps tendon (anterior aspect of the shoulder joint, 1cm below the coracoid process) or the supraspinatus tendon (acromial process).
- Acute shoulder pain (microcrystalline arthritis):
Shoulder pain appears suddenly with severe characteristics; pain causes insomnia, pain spreads to the entire shoulder, spreads to the neck, spreads down the arm, and sometimes down to the hand. Patients with severely reduced shoulder mobility often have their arms close to their bodies, unable to perform passive shoulder movements, especially abduction (pseudo-stiff shoulder due to pain). The shoulder is red and hot. A lumpy mass corresponding to the inflamed bursa can be seen in the front of the arm. There may be a low-grade fever.
- Pseudo-paralysis of the shoulder (rotator cuff rupture):
Severe pain with a cracking sound and a bruise may appear in the upper front of the arm a few days later. Pain is associated with obvious limitation of movement. Examination shows loss of active shoulder elevation, while passive movement is entirely normal, with no neurological signs. If the long bundle of the biceps tendon is ruptured, examination shows a muscle rupture in the front of the arm when flexing the forearm against resistance.
- Stiff shoulder (frozen shoulder):
Mechanical shoulder pain, sometimes at night. Examination: limited shoulder movement in both active and passive movements. Restrict movements, especially abduction and external rotation. When observing the patient from behind, when the patient raises his arm, the scapula moves as a unit with the humerus.

Diagnosis
Doctors need to carefully examine the functional and physical symptoms and test methods to diagnose the clinical manifestations of the disease accurately. Paraclinical tests may be required to coordinate diagnosis and treatment, such as:
- Shoulder X-ray: used to examine lesions in the shoulder joint, degenerative conditions, and lesions of ligaments and tendons around the shoulder joint.
- Shoulder ultrasound: mainly used to examine lesions of tendons, ligaments, and other soft tissue lesions.
- Magnetic resonance imaging (MRI): can detect early small tears and ruptures in the tendons.
- Computed tomography (CT-scan): usually indicated when the patient cannot have an MRI.
- Blood tests: blood tests for biological inflammatory syndrome are often negative.
Differential diagnosis
- Shoulder pain is caused by other causes such as angina, lung apex lesions, cervical spine root pain, etc.
- Bone pathology: Avascular necrosis of the upper end of the humerus.
- Joint diseases: Purulent arthritis, tuberculosis arthritis, crystal-induced inflammation such as gout or calcification of articular cartilage, rheumatoid arthritis, ankylosing spondylitis, etc.
Treatment
If not diagnosed and treated early, simple and acute shoulder pain will lead to persistent pain and limited shoulder joint movement, significantly affecting the patient’s quality of life and, over time, will lead to frozen shoulder peri arthritis or tendon rupture.
- Treatment principles
Treatment of shoulder periarthritis includes acute treatment and maintenance treatment. Combining many measures, such as internal medicine, surgery, physical therapy, and rehabilitation, is necessary.
- Non-drug treatment
- Non-drug treatments have shown outstanding local effectiveness and have limited the side effects of drugs.
- In addition, patients must change their lifestyle and activities and avoid activities that put weight on the shoulder and bad postures, such as reaching for objects, etc.
- Acupuncture helps to relieve acute and chronic pain effectively.
- Acupressure massage helps to stretch muscles, increase muscle nutrition, and reduce pain.
- Physical therapy methods include electrotherapy, shortwave, ultrasound therapy, and shoulder joint exercise.
- Drug treatment
- Pain relievers according to the Ministry of Health’s steps with Paracetamol/Codein
- NSAID pain relievers (Meloxicam, Diclofenac, Celecoxib)
- Osteoarthritis-reducing drugs (Glucosamine, Diacerein)
- Corticoid anti-inflammatory drugs (Methylprednisolone, Betamethasone)
- Corticoid injections at the joint
- Surgical treatment
- Indicated for pseudo-paralysis, especially in young people with ruptured tendons in the shoulder joint due to trauma. Surgery to reconnect the ruptured tendon. In the elderly (> 60 years old), tendon rupture due to degeneration, surgery should be indicated with caution.
- Periodic re-examination is required after 1-3 months, depending on the condition of the disease. Ultrasound of the shoulder joint can be performed to check the condition of the tendon, tendon sheath, and shoulder joint.
Prevention
Avoid overexertion, excessive movements, or lifting the arm above the shoulder.
Avoid injuries to the shoulder joint, especially injuries during movement and sports.
Detect and treat simple shoulder pain and acute shoulder pain early.
Practice shoulder joint exercises with the correct range of motion.