Definition
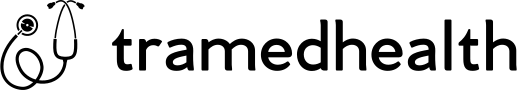
Cervical scapulohumeral syndrome is, in essence, a group of symptoms related to cervical spine diseases. Additionally, it is accompanied by dysfunction of the roots, nerves of the cervical spine, and/or the cervical cord. However, it is not associated with inflammatory pathology.
Moreover, common clinical manifestations include pain in the neck, shoulder, and arm. Furthermore, this pain is often accompanied by sensory disturbances. Additionally, motor disturbances may occur in the areas supplied by the affected cervical nerve roots.
Causes
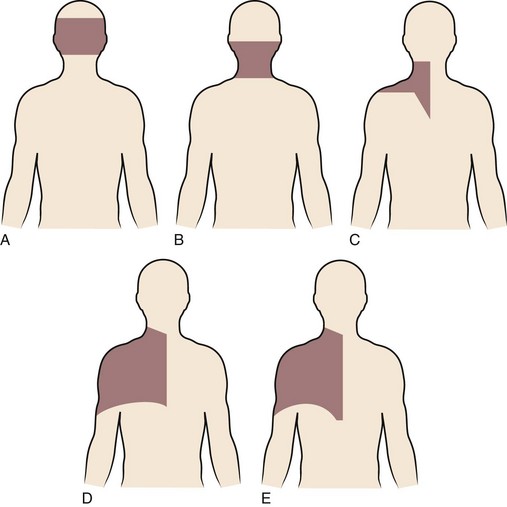
- The most common cause, accounting for 70-80% of cases, is cervical spondylosis. This condition involves the degeneration of the intervertebral and lateral interarticular joints. As a result, the foramen narrows, which compresses the cervical spinal nerve roots or nerves at the foramen.
- Cervical disc herniation (20-25%), alone or in combination with cervical spondylosis.
- Other rare causes include trauma, tumors, infections, osteoporosis, spondylitis, and paraspinal soft tissue disease.
- In some cases, cervical shoulder-arm syndrome is due to cervical spine disease itself, causing neck pain and radiating to the shoulder or arm, without cervical nerve root disease.
Symptom of Cervical Scapulohumeral Syndrome
Depending on the cause, severity, and stage of the disease, the patient may have more or less of the following symptoms and syndromes:
- Cervical spine syndrome:
- Pain in the neck area can start acutely after trauma, after excessive neck movement, or naturally after waking up. The pain can also appear slowly, dull, and chronically.
- Limited movement of the cervical spine may be accompanied by signs of torticollis, often seen in acute cervical spine pain.
- Pain points in the cervical spine when pressing on the posterior spines next to the cervical spine corresponding to the nerve roots.
- Nerve root syndrome:
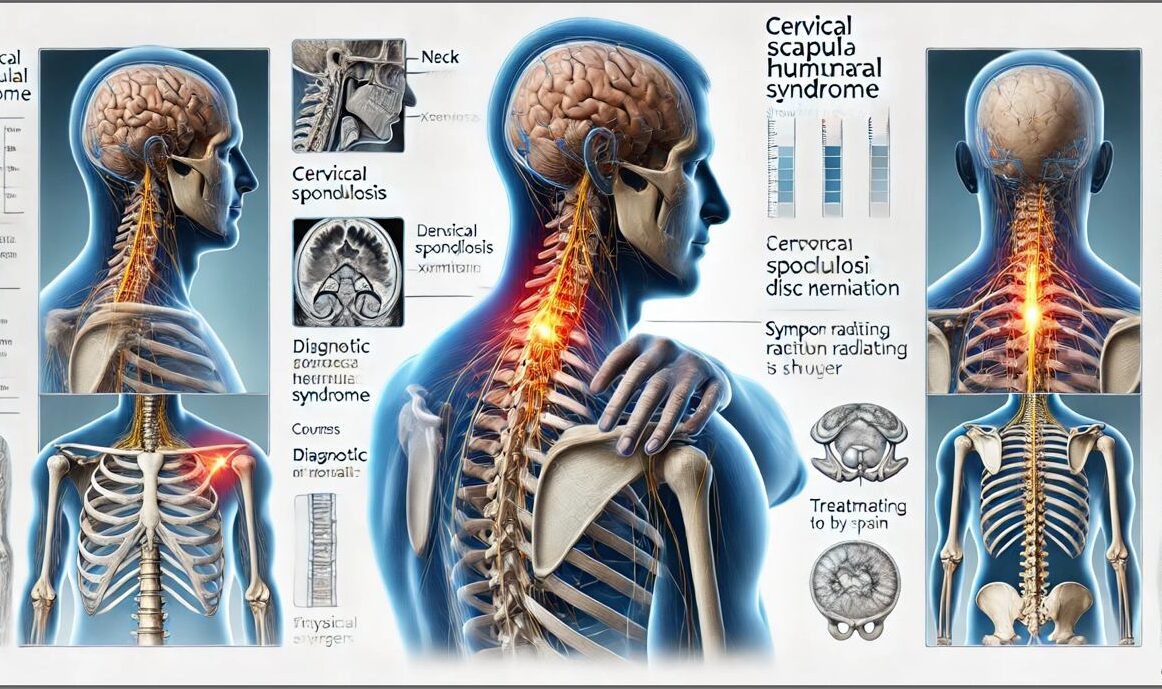
- Pain in the neck area spreads to the occipital region and down to the shoulder arm or hand; the clinical manifestation is cervical shoulder syndrome or shoulder arm syndrome. Pain often increases when turning the head or bending the neck towards the painful side.
- Motor and sensory disorders of the root type: Muscle weakness and sensory disorders such as burning, tingling, numbness in the shoulder, arm, or hand and fingers.
- Some tests to assess cervical nerve root damage are bell signs, Spurling tests, shoulder abduction tests, and neck extension tests.

- Cervical cord syndrome:
- Due to disc protrusion or herniation causing progressive compression of the cervical cord over a long period of time.
- Early manifestations are signs of numbness and loss of dexterity in both hands, muscle atrophy of both arms, difficulty walking, and rapid fatigue. In the late stage, depending on the location of the lesion, central paralysis of the limbs may be seen, peripheral paralysis of both arms, central paralysis of both legs and impaired bladder and bowel reflexes.
- Other symptoms:
- Vertebrobasilar artery syndrome: Occipital headache, dizziness, tinnitus, blurred vision, sometimes transient visual loss, loss of balance, fatigue.
- There may be autonomic nervous system disorders: Pain accompanied by tinnitus, visual disturbances, and vascular disorders in the occipital shoulder or arm area.
- When there are systemic symptoms such as fever, chills, night sweats, weight loss, etc., special attention must be paid to excluding malignancy and infection.
Diagnosis
The doctor needs to clearly exploit the patient’s medical history and symptoms to make the most accurate diagnosis and may also recommend paraclinical tests to support diagnosis and treatment, such as:
- Regular X-ray: Need to take straight, tilted, and 3/4 oblique positions. An X-ray can detect cervical spine lesions due to trauma, degeneration, stenosis of the foramen, vertebral collapse due to osteoporosis, bone destruction due to malignancy, etc.
- Magnetic resonance imaging (MRI): MRI is often indicated when the patient has prolonged pain (>4-6 weeks), increasing pain, progressive nerve damage, signs of cervical myelopathy, or warning signs suggesting malignancy or infection.
- Computed tomography (CT Scan) alone or with contrast myelography: CT scan alone can be indicated when MRI is not available, or MRI is contraindicated.
- Electromyography: Can help detect nerve-origin lesions and differentiate cervical myelopathy from peripheral nerve and root pathology.
- Blood tests: Have little diagnostic value in cervical spine and disc pathology, causing mechanical compression. In diseases such as tumors, inflammation, and infection, changes may be seen in some tests, such as peripheral blood cells, erythrocyte sedimentation rate, CRP, alkaline phosphatase, serum protein electrophoresis, etc.
- Bone scintigraphy: When suspected of metastatic cancer or vertebral disc inflammation, osteomyelitis.
Treatment
Treatment principles
- Treat symptoms combined with addressing the cause if possible.
- Combine drug treatment with physical therapy, rehabilitation, and other non-drug measures.
- Indicate surgical treatment when necessary.
Non-drug treatment
- Patients need to change their living and working habits (sitting position, using a computer, etc.).
- In the acute phase, when there is severe pain or after trauma, the cervical spine can be relatively immobilized with a soft neck brace.
- Acupuncture can effectively relieve pain in both acute and chronic conditions.
- Acupressure massage helps relieve pain, relax muscles, and increase circulation to the neck and shoulder area.
- Exercise the cervical spine, shoulders, and arms with appropriate exercises.
- Physical therapy: Heat therapy, electrical stimulation, ultrasound therapy, spinal traction.
Drug treatment
- Can use antipyretic analgesics (Paracetamol), NSAID anti-inflammatory drugs (Diclofenac, Meloxicam)
- Muscle relaxants (Eperisone)
- Nerve pain relievers (Gabapentin, Pregabalin), Vitamin 3B
- Corticosteroid anti-inflammatory drugs (Prednisolone, Methylprednisolone)
- Epidural corticosteroid injection or injection into the posterior inter-articular joint next to the cervical spine
- Interventional pain relief procedures: Selective nerve root blockade
Surgical treatment
- Some indications: Severe pain but medical treatment has little effect, there is severe and progressive nerve damage, and there is significant cervical spinal cord compression.
- Some main surgical methods: Spinal correction to relieve nerve compression at narrowed foramina, remove herniated disc nucleus pulposus, fuse and stabilize the spine.
Prevention
It is necessary to maintain a proper head and neck posture in daily life, work, study, and sports activities; avoid sitting postures, working postures that cause excessive neck bending, neck arching or neck rotation for a long time, avoid sitting or standing for too long, pay attention to the appropriate sitting posture and chair.
Perform appropriate cervical spine exercises to strengthen the muscles of the neck, chest, and shoulders, as well as prevent the neck muscles from becoming tired or stiff.