Definition of Alzheimer’s disease
Alzheimer’s disease is a leading cause of dementia, resulting in memory loss and cognitive dysfunction, significantly impacting the quality of life and work of affected individuals.
The prevalence of Alzheimer’s disease increases with age, ranging from approximately 5% in individuals under 75 years old to 40-50% in those over 85 years old. Moreover, Alzheimer’s disease is associated with a substantial treatment budget and imposes significant physical and mental burdens on patients and their families.
Causes
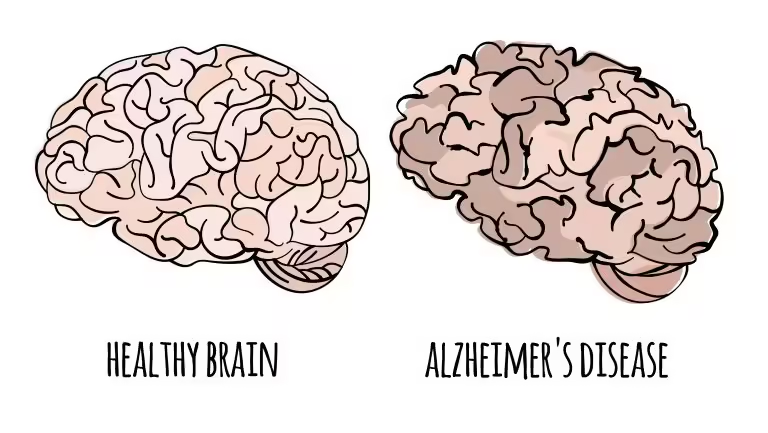
Alzheimer’s disease results from a degenerative process that leads to the death of neurons. The two primary pathological hallmarks are Amyloid plaques and neurofibrillary tangles:

- Formation of amyloid β-42: The amyloid β-42 product polymerizes into toxic oligomers that induce inflammation of neuronal cell membranes, subsequently activating abnormal Tau protein processes within cells, and ultimately contributing to neuronal death.
- Formation of neurofibrillary tangles: Phosphorylated Tau proteins aggregate to form neurofibrillary tangles (NFTs) that deposit in the cell body and proximal axons. Consequently, this process disrupts cellular function and leads to cell death.
Symptoms of Alzheimer’s disease
The clinical symptoms of dementia are diverse and vary depending on the stage of the disease.
Cognitive impairment manifestations
- Memory decline: This is the characteristic, early, typical, and prominent symptom of dementia. Furthermore, as the disease progresses, memory impairment becomes increasingly severe.
- Disorientation: Disorientation, particularly regarding space and geography, is a significant symptom in the clinical presentation of dementia.

Other cognitive function impairments:
- Aphasia: This may present as expressive or receptive aphasia.
- Agnosia: The ability to recognize and name objects or people is reduced or lost, even though the sensory organs remain intact.
- Functional impairment: Impaired ability to carry out activities despite intact motor functions.
- Reduced abstract thinking, calculation ability, planning, creativity, decision-making, coordination, and the ability to follow through with complex tasks.
Non-cognitive symptoms
- Psychotic symptoms: Delusions are present in 30-40% of dementia patients. Hallucinations occur in 20-30% of patients. Capgras syndrome may also be observed.
- Emotional disturbances: Depression and anxiety are found in 40-50% of dementia patients.
- Personality changes: Patients may become withdrawn; additionally, some may become stingy, suspicious, irrationally jealous, childlike, or neglectful in their appearance, with a tendency towards hoarding unclean objects.

Behavioral disturbances: Agitation during the night, eating, and toileting behavior disturbances.
Other symptoms:
- Focal neurological signs may be present in dementia.
- Sundown syndrome.
- Confusion, agitation, and falls.
The average life expectancy for Alzheimer’s patients is approximately 5-15 years, depending on the age of disease onset.
Diagnosis
Diagnostic Criteria for Alzheimer’s Disease (ICD-10 or DSM-IV):
- Symptoms persist for at least six months.
- Memory impairment: particularly a decline in acquiring new information and recalling previously learned knowledge.
- Impairment in other cognitive functions (at least one of the described manifestations is required).
- Non-cognitive symptoms may be present.
- Symptoms occur without accompanying disturbances in consciousness.
- Characteristics typical of Alzheimer’s disease.
Laboratory and Imaging Studies: Additional diagnostic studies may be indicated depending on the specific case:
Psychological testing:
- Cognitive assessments (MMSE, GPCOG, Mini-Cog, ADAS-Cog, Wechsler).
- Depression assessments (Ham-D, Beck, GDS).
- Anxiety assessments (Ham-A, Zung).
- Sleep disorder assessments (PSQI).
- Personality assessments (EPI, MMPI).
Blood tests, biochemical analysis, and urinalysis.
Imaging studies: Brain CT, brain MRI, SPECT, PET, and fMRI are used to support diagnosis and exclude cerebrovascular disease and other space-occupying lesions. Additionally, abdominal ultrasound, chest X-ray, and echocardiography are performed to detect comorbidities or complications.
Functional testing: EEG, cerebral blood flow studies, ECG, transcranial Doppler ultrasound.
Differential Diagnosis:
- Depressive disorder.
- Delirium.
- Amnestic disorder due to medical conditions: thyroid disease, vitamin B12 deficiency.
- Other primary dementias (such as vascular dementia, Pick’s disease, Lewy body dementia, Creutzfeldt-Jakob disease, Huntington’s disease, or dementia in Parkinson’s disease).
- Toxic states.
Treatment
Treatment Principles
Assess the severity of dementia, particularly the patient’s ability to live independently, to develop an appropriate treatment plan that addresses both physical and mental health. Establish care and management plans for the patient in hospitals, nursing homes, and the community while also planning to support the patient’s family in improving their quality of life.
Pharmacological treatment:
- Cognitive decline treatment: Donepezil, Rivastigmine, Galantamine
- Antipsychotics: Olanzapine, Clozapine, Haloperidol
- Antidepressants: Sertraline, Fluoxetine, Mirtazapine
- Mood stabilizers: Carbamazepine, Oxcarbazepine
Non-pharmacological treatment:
- Psychotherapy
- Physical and occupational therapy: Rehabilitation of motor functions and speech therapy
- Assistance with daily activities
- Social management
- Support for caregivers
Prevention
There are no specific preventive measures for the disease. However, some general measures include:
- Avoiding tobacco, alcohol, and stimulants.
- Furthermore, preventing and treating hypertension, hyperlipidemia, and diabetes.
- In addition, maintaining a balanced diet rich in fruits and vegetables, with reduced sugar and saturated fats.
- Finally, engaging in regular physical and cognitive activities.