Definition of Knee Osteoarthritis
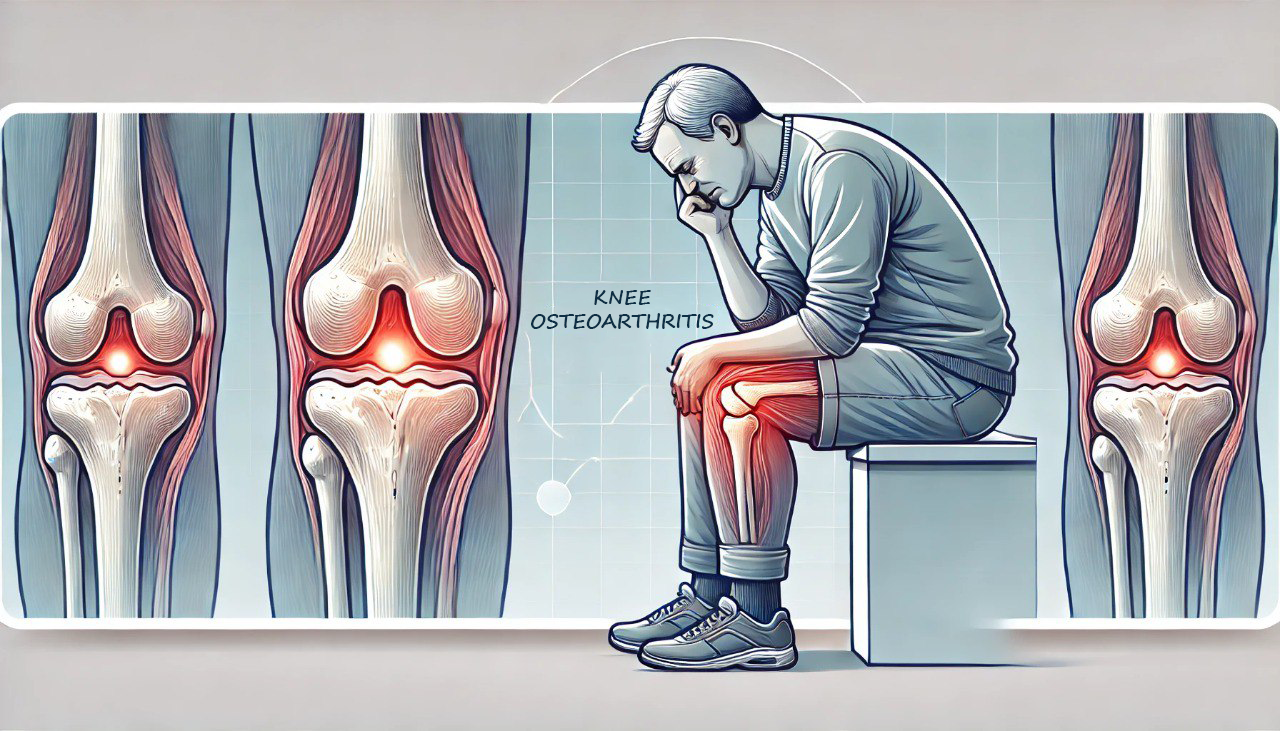
Knee osteoarthritis results from a fundamental biological process that disrupts the balance between the synthesis and degradation of cartilage and subchondral bone.
Various factors, including genetic, developmental, metabolic, and traumatic influences, can initiate this imbalance.
Consequently, the final manifestation of osteoarthritis involves a range of changes: morphological, biochemical, molecular, and biomechanical alterations in both the cells and matrix of the cartilage.
These changes ultimately lead to degeneration, fissures, and loss of articular cartilage, as well as subchondral sclerosis, osteophyte formation, and damage to the subchondral cartilage.
Causes
- Primary osteoarthritis
The main cause is that it appears late, usually in people over 60 years old, can be in one or more joints, and progresses slowly. In addition, there may be genetic factors, endocrine and metabolic factors (menopause, diabetes, …) that can increase the degenerative condition.
- Secondary osteoarthritis
The disease occurs at all ages; the cause can be due to:- After injuries that cause the joint axis to change (joint fracture, misalignment, etc.)
- Congenital abnormalities of the knee joint axis: the knee rotates outward (genu valgum); the knee rotates inward (genu varum); the knee is hyperextended (genu recurvatum)
- After other inflammatory lesions in the knee joint (rheumatoid arthritis, gout)
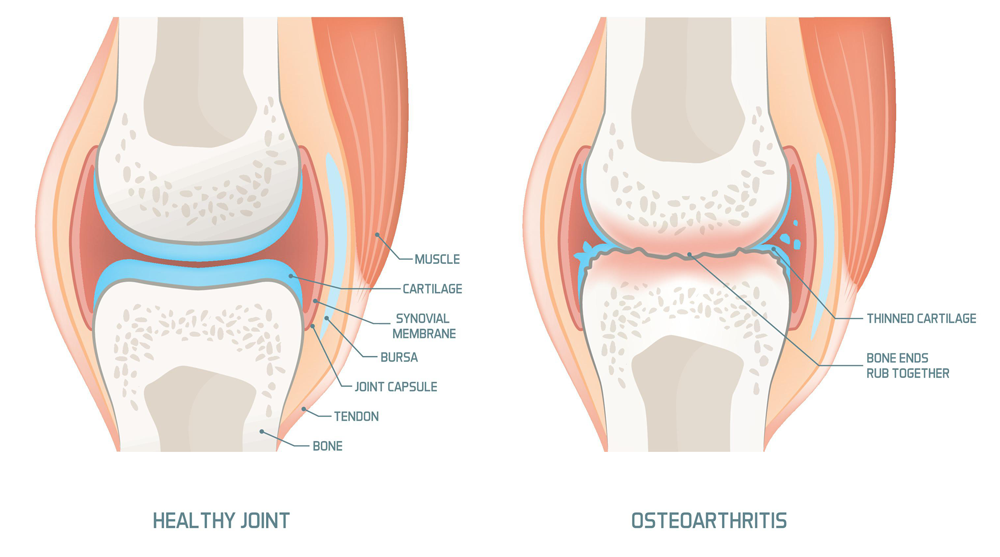
Symptoms of Knee Osteoarthritis
- Pain around the knee joint is a typical symptom; depending on the acute or chronic phase, it can be severe or dull. Pain increases when walking and decreases when resting.
- Limited movement of the knee joint, reduced knee flexion range.
- Crackling of the knee when flexing and extending.
- Knee joint deformity, misalignment.
- Easily fatigued when standing and walking for a long time.
- Knee joint may swell.
Diagnosis
Apply the American College of Rheumatology (ACR) diagnostic criteria, 1991.
Paraclinical support for diagnosis and treatment:
- Knee X-ray: images of bone spurs, joint space narrowing, and bone head hyperplasia.
- Joint ultrasound: assess the condition of narrowing of the joint space, bone spurs, and joint effusion, measure the thickness of articular cartilage and synovial membrane, and detect degenerative cartilage fragments that have detached into the joint cavity.
- Magnetic resonance imaging (MRI): This method can observe the image of the joint entirely in three dimensions and detect damage to articular cartilage, ligaments, and synovial membrane.
- Arthroscopy: the arthroscopy method directly observes degenerative lesions of articular cartilage at different levels (according to Outbright’s four-degree division) through arthroscopy combined with synovial membrane biopsy to perform cell testing to differentiate from other joint diseases.
- Blood and biochemical tests: Normal erythrocyte sedimentation rate.
Differential diagnosis
- Rheumatoid arthritis: differential diagnosis when only the knee joint is affected, significantly when only one joint is affected: inflammation in the joint and clear biological signs of inflammation (increased erythrocyte sedimentation rate, increased CRP, etc.), and there may be a positive rheumatoid factor—usually diagnosed by endoscopy and synovial membrane biopsy.
- Gouty arthritis: acute attacks of gouty arthritis and osteoarthritis can have similar symptoms; it is necessary to distinguish clearly to avoid confusion and treat them appropriately.

Treatment
- Treatment principles
- To manage knee osteoarthritis effectively, focus on pain relief during progression.
- Additionally, aim to restore joint mobility and limit or prevent joint deformities.
- Moreover, be cautious to avoid unwanted drug side effects, paying attention to drug interactions and associated diseases, particularly in the elderly.
- Ultimately, improving the quality of life for patients remains a key goal.
- Non-drug treatment
- Change your lifestyle by avoiding standing or sitting for prolonged periods. Moreover, exercise moderately and appropriately to maintain joint health.
- In addition, acupuncture can significantly improve symptoms such as pain, weakness, and knee fatigue.
- Similarly, acupressure massage helps relieve pain, relax muscles, and enhance circulation in the knee area.
- Furthermore, physical therapy methods like electrotherapy, ultrasound, and infrared therapy are highly effective for managing knee osteoarthritis.
- Drug treatment
- Pain relief options include: Paracetamol and Tramadol.
- Additionally, non-steroidal anti-inflammatory drugs (NSAIDs) such as Celecoxib and Piroxicam can be used.
- In contrast, topical anti-inflammatory drugs generally have fewer side effects compared to oral medications.
- Moreover, corticosteroids are not indicated for systemic use.
- For intra-articular injections, options include Hydrocortisone acetate, Hyaluronic acid (AH) in the form of hyaluronate, Betamethasone, and Methylprednisolone.
- Furthermore, slow-acting anti-degenerative drugs such as Piascledine and Glucosamine sulfate are available.
- Autologous platelet-rich plasma (PRP) treatment involves taking venous blood, adding an anticoagulant, centrifuging to separate plasma, and then injecting 6ml-8ml of PRP into the knee joint.
- Additionally, stem cell transplantation uses stem cells extracted from autologous adipose tissue (Adipose-derived Stem-Cell-ADSCs) or autologous bone marrow.
- Surgical treatment
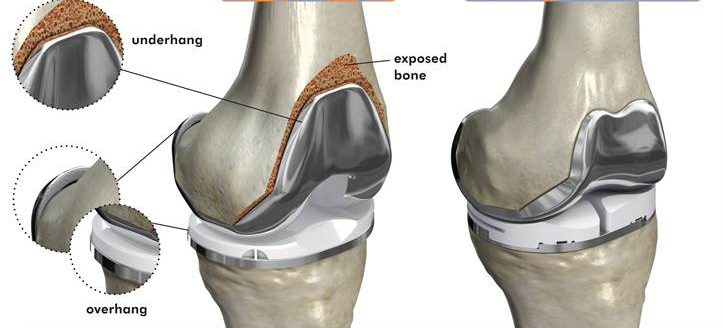
- Arthroscopic treatment options include debridement, shaving, and joint lavage. Additionally, drilling to stimulate bone formation (known as microfracture) and cartilage cell transplantation are used to address cartilage damage.
- On the other hand, artificial joint replacement surgery is typically indicated in severe, progressive cases where there is significant loss of motor function. This procedure is usually applied to patients over 60 years old and may involve partial or total knee replacement.
Prevention
To prevent knee osteoarthritis, it is essential to maintain a healthy weight and prevent obesity. Additionally, having a reasonable exercise regimen can help protect joints from overload and reduce the risk of developing the condition. Moreover, early detection and treatment of orthopedic joint deformities, such as joint misalignment or knee joint curvature (internal or external), are crucial for preventing the progression of knee osteoarthritis.