Definition of Sciatica Pain
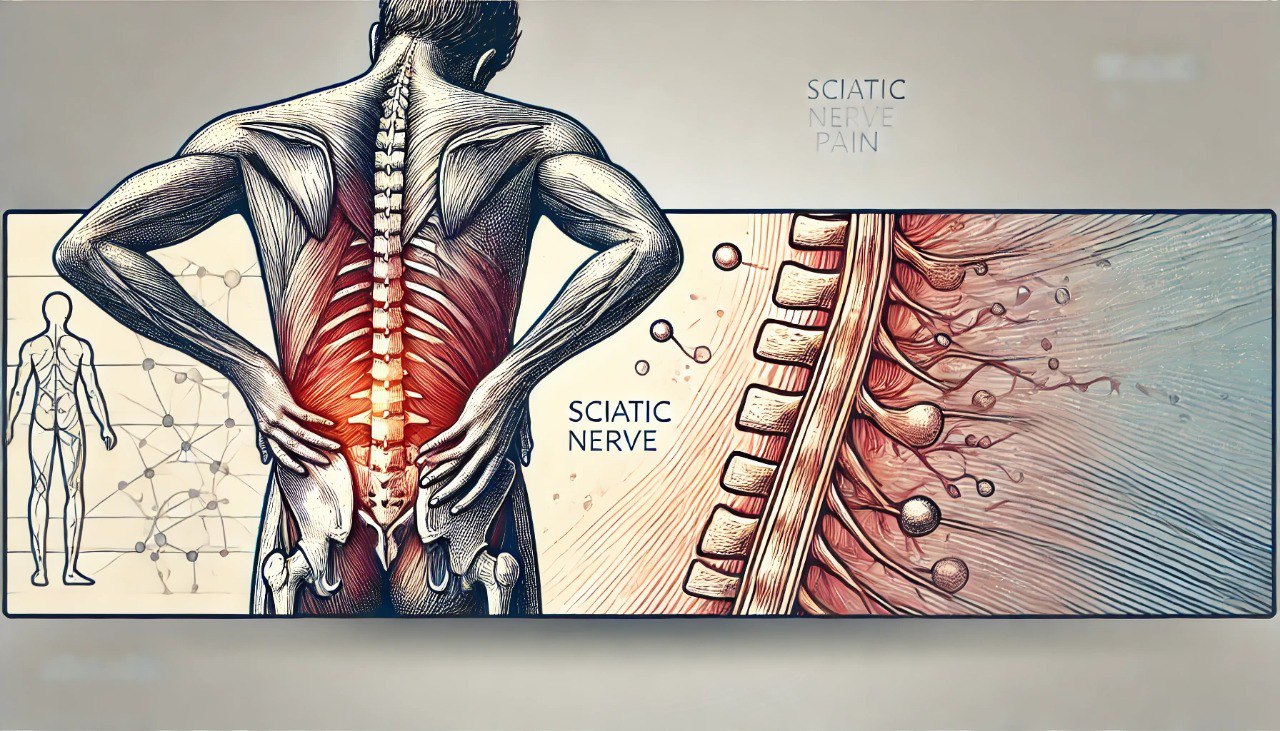
Sciatica pain typically presents as pain radiating along the sciatic nerve, starting in the lumbar spine and extending to the outer thigh, the front and outer calf, the outer ankle, and the toes. The direction in which the pain spreads can vary depending on the specific location of the lesion.
Causes
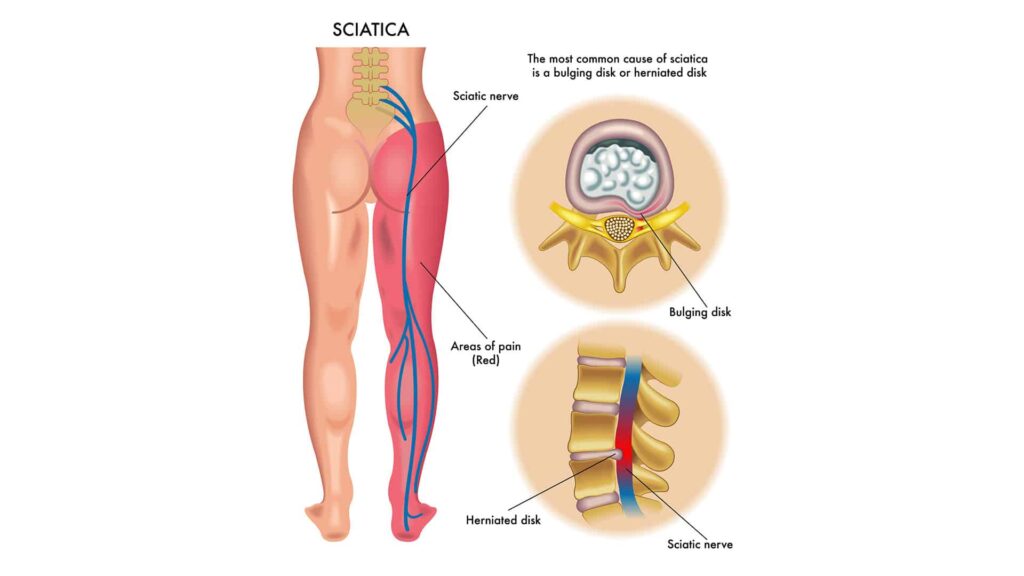
The leading cause of sciatic nerve root compression is disc herniation, most commonly at the L4-L5 or L5-S1 disc, which causes compression of the corresponding L5 or S1 root. Additionally, conditions such as spondylolisthesis and lumbar spine degeneration, leading to lumbar spinal stenosis, are also significant contributors. Moreover, these groups of degenerative causes can often be combined.
On the other hand, less common causes include spondylodiscitis, vertebral body injury (usually due to tuberculosis, bacteria, or tumors), trauma, and pregnancy.
Symptom of Sciatica Pain
- Pain along the sciatic nerve often manifests as pain in the lumbar spine radiating to the outer thigh, front and outer calf, outer ankle, and toes. However, in some cases, pain may occur from the buttocks to the legs without any back pain, a condition known as Piriformis Syndrome.
- The pain may be continuous or intermittent. Typically, it is reduced by lying down to rest and exacerbated by walking. Furthermore, accompanying symptoms may include numbness, tingling, paresthesia, and decreased or lost sensation in areas controlled by the sciatic nerve. Additionally, muscle weakness may occur.
- In later stages, symptoms can progress to quadriceps atrophy, limited mobility, and spasticity of the paraspinal muscles.
Diagnosis
Based on the symptoms reported by the patient, the doctor needs to examine carefully to make a correct diagnosis and find the cause of sciatica syndrome.
Some tests that can be performed are:
- Valleix pain point system, positive bell sign.
- Positive Lasègue sign.
- Other signs with equivalent value to the Lasègue sign are the Chavany and Bonnet.
- Tendon reflexes: Patellar tendon reflex is reduced or lost in L4 root injury, Achilles tendon reflex is reduced or lost in S1 root injury.
Some paraclinical tests support diagnosis and treatment, such as:
- Tests for signs of inflammation in negative blood tests; average biochemical indices do not change. However, it is necessary to prescribe an inflammatory bilan test, a basic test to rule out diseases such as infection and malignancy, and necessary when prescribing medication.
- Routine lumbar spine X-rays have little value in diagnosing the cause. Most cases of conventional X-rays are standard or show signs of lumbar spine degeneration or spondylolisthesis. Conventional X-rays are indicated to rule out specific causes (inflammation of the vertebral disc, destruction of the vertebral disc due to cancer, etc.).
- Magnetic resonance imaging (MRI) of the lumbar spine: to accurately determine the type of lesion as well as the location of the herniated mass, the extent of the herniated disc, and can detect other rare causes (inflammation of the vertebral disc, tumors, etc.).
- Computed tomography (CT) scan: only indicated when MRI is unavailable.
- Electromyography: helps detect and assess damage to nerve roots.
Differential diagnosis:
We need to differentiate from cases of pseudo-sciatica.
- Femoral neuralgia, femoral cutaneous neuralgia, obturator nerve pain.
- Hip joint pain due to inflammation, necrosis, degeneration, trauma.
- Sacroiliitis, inflammation, and abscess of the iliopsoas muscle.
Treatment
If not detected and treated early, sciatica can eventually lead to lower limb movement disorders, potentially causing partial or complete paralysis of the lower limbs, as well as lower limb sensory disorders and sphincter (circular) disorders.
Treatment principles
- Treatment according to the cause (most commonly lumbar disc herniation).
- Pain relief and rapid recovery of movement.
- Medical treatment for mild and moderate cases.
- Surgical intervention when there are complications related to movement and sensation.
- Sciatica due to malignant causes: spinal decompression treatment combined with specialized treatment.
Non-drug treatment
- Lie on a hard bed, and avoid sudden, muscular movements, heavy lifting, standing, and sitting for too long.
- Change your lifestyle, exercise, rest properly, and wear a back support belt.
- Acupuncture helps to effectively relieve local pain as well as neurological symptoms in the legs
- Acupressure massage helps to relax muscles, reduce pain, and increase circulation in the areas controlled by the sciatic nerve.
- Physical therapy: Electrotherapy, shortwave, ultrasound therapy, electromagnetic field, exercise therapy, hot and cold compresses, infrared radiation, etc.
Drug treatment
Pain relievers. Depending on the level of pain, use one or a combination of the following pain relievers:
- Pain relievers: Paracetamol/Codein/Tramadol.
- Non-steroidal anti-inflammatory drugs (NSAIDs): Meloxicam, Diclofenac, Celecoxib
- In cases of severe pain, it may be necessary to use opium preparations such as morphine.
- Muscle relaxants: Eperisone, Tolperisone.
- Neuropathic pain relievers: Gabapentin, Pregabalin, vitamin 3B.
- Corticoid anti-inflammatory drugs: Methylprednisolone, Prednisolone.
Surgical treatment
Indicated when medical treatment fails or in cases of severe compression (cauda equina syndrome, spinal stenosis, lower limb paralysis, etc.), muscle atrophy.
- Discectomy: removal of a small part of the herniated disc causing nerve compression. Indicated after three months of ineffective pain treatment. In cases where the patient has complications of limited mobility and severe sensory disturbances, surgery is needed sooner.
- Posterior vertebral orchiectomy: indicated for sciatica due to spinal stenosis; this method makes the spine unstable and prone to recurrence.
- In cases of spondylolisthesis causing severe nerve compression: fixation by spinal rigidification, spinal screw fixation.
Prevention
Sciatica can be prevented entirely at home in straightforward ways as follows:
First and foremost, change your lifestyle and activities to avoid bending over, incorrect posture, and carrying heavy objects. Moreover, keep your spine upright when sitting for long periods or driving; you can also wear a back support belt. Additionally, practice moderate physical exercises such as swimming or yoga to increase the endurance and flexibility of your back muscles. Finally, incorporate exercises specifically designed to strengthen the back muscles.